The Department of Anaesthesia at CMC Vellore strives to provide outstanding patient care and the finest education for medical students and residents, with its team of accomplished faculty and world-class infrastructure. Each year, the department provides services for around 47,000 procedures within 58 operating rooms and 13 NORA, under a broad spectrum of medical and surgical needs.
The speciality of Anaesthesia is changing rapidly owing to the complexity of the cases seen and the technologies available for patient care. There are new demands placed upon practitioners concerning the skills necessary for the management of clinical practice, far exceeding those which were needed just a decade ago. We currently cover 71 anaesthesia areas, with 220 cases per day.
We have 67 consultants and 99 residents and provide anaesthetic care for all specialities including Cardiothoracic Surgery, Neurosurgery, Paediatric Surgery, major oncology surgeries (Urology, Gynaecology, Orthopaedics, Colorectal, Upper GI, Hepatobiliary, endocrine surgery), joint replacement and spine surgeries, bariatric procedures, major plastic and reconstructive surgeries, Trauma Surgery and airway procedures. We also provide anaesthetic cover in remote locations for diagnostic procedures – Gastroscopy, MRI, DSA, CT, RT, lithotripsy, ECT, etc.
The Department of Anaesthesia provides expert anaesthesia care for the full spectrum of medical and surgical indications seen at a major tertiary care academic institution and Level 1 trauma centre.
General intra-operative care is divided into procedure-related areas: cardiovascular and thoracic, neurological, genitourinary, general surgical, otorhinolaryngological (ENT), Dental, ophthalmologic, orthopaedic, gynaecologic, paediatric, including liver and kidney transplants.
Short therapeutic procedures or diagnostic studies such as special X-rays, MRIs and interventional radiology-related procedures, endoscopy and related procedures, and electro-convulsive therapies that need an anaesthesiologist’s presence and special skills are also provided.
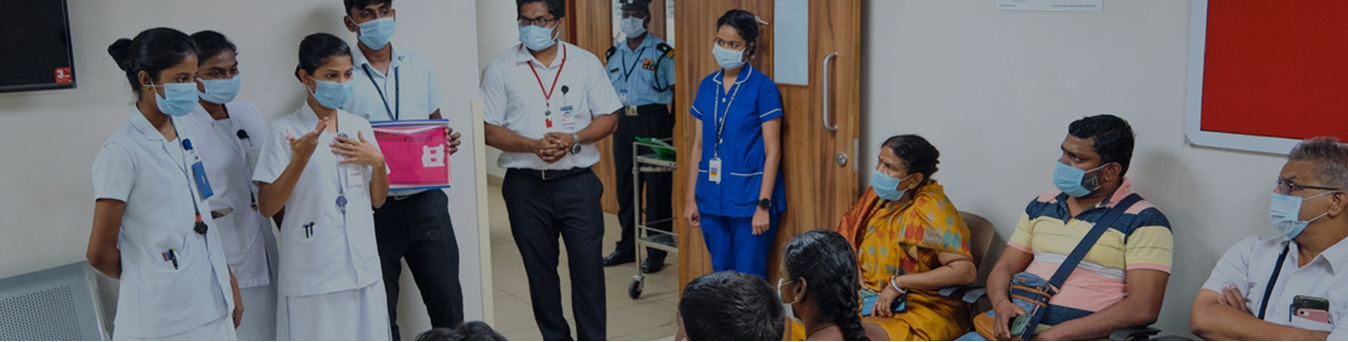
Pre- Anaesthesia Clinic
Pre- Anaesthesia Clinic was established in 2008 by Dr. Sarah Ninan. We screen about 150 cases per day. Patients are educated about anaesthesia with the help of videos, flashcards and patient information leaflets. Labour Analgesia and Acute Pain Services are also provided.
High-Risk Clinic (HRCA): started on 1st March 2021
The High-Risk Anaesthesia Clinic aims to evaluate, optimise, and provide perioperative care for patients with significant co-morbidities. Most developed countries have high-risk preoperative clinics to cater to this group and this has been shown to reduce morbidity. In this clinic, surgical as well as medical patients at higher risk of developing complications are comprehensively evaluated and interventions are efficiently coordinated and completed in the weeks leading up to the surgery. This new facility is functioning in the Alpha Clinic, Rooms 24 and 25.
Effective utilisation of an anaesthetic clinic depends on appropriate referral of “high-risk surgical patients”. Increased life expectancy and affordability of care have resulted in more elderly patients with multiple co-morbidities presenting for surgeries. Similarly, patients with significant co-morbidities, GUCH (Grown-up congenital heart disease – partially corrected), and Children with significant co-morbidities, present to the Pre-Anaesthesia Clinic (PAC) often immediately before surgery. This may result in last-minute cancellations or suboptimal outcomes. To achieve the best peri-operative outcome, anaesthetists must be part of the multidisciplinary team that optimise and manage these ‘high-risk patients’.
| COURSES | DURATION | ACCREDITATION | NO OF SEATS INTAKE |
| Post Doctoral Fellowship In Paediatric Anaesthesia | 1 Year | The Tamilnadu Dr. Mgr Medical University, Chennai | 1 |
| Post Doctoral Fellowship In Nerve Block & Pain Management | 1 Year | The Tamilnadu Dr. Mgr Medical University, Chennai | 1 |
| Post Doctoral Fellowship In Cardia Anaesthesia | 1 Year | The Tamilnadu Dr. Mgr Medical University, Chennai | 2 |
| Post Doctoral Fellowship In Advanced Clinical Anaesthesia And Perioperative Medicine | 1 Year | Cmc Vellore | 10 |
| Wfsa-Paediatric Anaesthesia Fellowship | 6 Months | Wfsa | 1 |
ALLIED HEALTH SCIENCES
| COURSES | DURATION | ACCREDITATION |
NO OF SEATS INTAKE |
| Bsc- Operation Theatre And Anaesthesia Technology | 3 Years | The Tamilnadu Dr. Mgr Medical University, Chennai | 11 |
| Diploma In Anaesthesia Technology And Critical Care Technology | 2 Years | Cmai | 15 |
The Head,
Department of Anaesthesia,
New Paul brand building,
7th Floor, Anaesthesia Office,
CMC Vellore Town Campus,
Ida Scudder Road, Vellore – 632004,
Tamil Nadu.
Email us :
anaesthesia@cmcvellore.ac.in
004162282105
Mon-Fri: 8 am to 4.30 pm
( Sat : 8 am to 12:30 pm)