Paediatric care at CMC started in 1928, when the first dedicated children’s ward was opened to provide specialised care. The Department of Child Health was established a few years later. Postgraduate paediatric training began in 1957, under the leadership of Dr. John Webb. Since then, over two hundred paediatricians have been trained, many of whom are faculty in eminent institutions around the world. Research has always been a vital component and the Department is renowned for ground-breaking work in various illnesses.
Over the years, the Department has grown under the guidance of Dr. Malati Jadhav, Dr. Sheila Pereira, Dr. Raghupathy and Dr. Chellam Kirubakaran. Today, the department of Child Health has six units – three general Child Health units, Neoanatology, Developmental Paediatrics and the Paediatric Intensive Care Unit.
Each of the Child Health Units in addition to general paediatric work have their own areas of expertise. Child Health Unit One has specialty interests in Paediatric Endocrinology, Hemato-Oncology and Infectious Diseases. The unit also supervises the Well Baby Clinic. Child Health Unit Two offers services in Paediatric Nephrology and Paediatric Rheumatology. Child Health Unit Three looks after Respiratory Medicine, Asthma and Adolescent Health (Read about Project Yuva under Adolescent Medicine). The Emergency Service which complements the work of the Child Health Unit receives acutely ill children who require prompt stabilisation and resuscitation. The Child Health units are committed to providing the highest quality of paediatric care, training undergraduate and post-graduate students, and net working with primary care doctors.
The Neonatology unit is the largest perinatal centre in the region and is internationally acclaimed for specialty training. The dedicated team of professionals offers comprehensive care for babies with complex needs using state-of-the-art technology.
Developmental Paediatrics Unit is one of the first teaching units of its kind in the country. The multi-disciplinary team provides consultation, assessment and assistance to children with different neuro-developmental needs. The Unit offers training to undergraduate and post-graduate students and is involved in research in various developmental issues.
Paediatric Intensive Unit (PICU) is a multi-disciplinary 11-bed unit that provides the highest level of care to critically ill children with medical and surgical problems.
Other units which are committed to looking after children include Paediatric Neurology which is a sub unit of the Department of Neurological Sciences, Paediatric Surgery, Child and Adolescent Psychiatry Unit, which is attached to the Mental Health Centre and Paediatric Occupational and Physical Therapy. Paediatric Nursing has emerged as a separate specialty since 1969 when post-graduate (MSc) programme commenced. Keeping with the times, the Paediatric Nursing department offers specialty training to look after children with special needs.
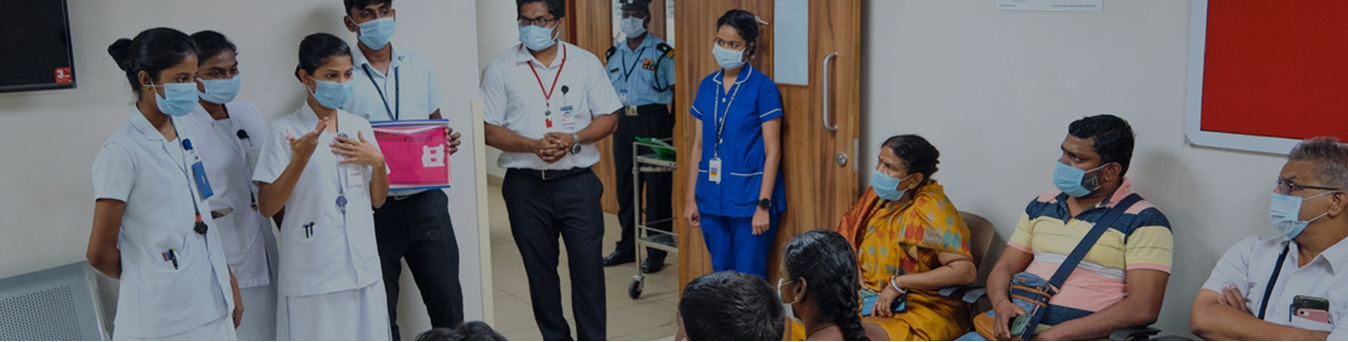
The Child Health units are committed to providing the highest quality of paediatric care, training undergraduate and postgraduate students, and networking with primary care doctors. Each of the Child Health Units in addition to general paediatric work has its areas of expertise.
Child Health Unit Two offers services in Paediatric Nephrology and Paediatric Rheumatology.
The Emergency Service which complements the work of the Child Health Unit receives acutely ill children who require prompt stabilisation and resuscitation.
The Neonatology Unit is the largest perinatal centre in the region and is internationally acclaimed for speciality training. The dedicated team of professionals offers comprehensive care for babies with complex needs using state-of-the-art technology.
Developmental Paediatrics Unit is one of the first teaching units of its kind in the country. The multi-disciplinary team provides consultation, assessment and assistance to children with different neuro-developmental needs. The Unit offers training to undergraduate and postgraduate students and is involved in research on various developmental issues.
Paediatric Nephrology
The Paediatric Nephrology subspecialty in Christian Medical College, as a subdivision of Pediatrics, was established in 2002. We provide outpatient and inpatient services and have facilities for the diagnosis and management of complicated renal diseases. Support is given to the Intensive care unit, Pediatric urology and other subspecialties of Paediatrics. For critically ill children with renal failure, haemodialysis, peritoneal dialysis, plasmapheresis and CRRT are provided. Maintenance dialysis programmes- both CAPD and Haemodialysis are available and we have a growing renal transplant programme.
Read more about the Paediatrics
Nephrology Unit:
Overview,
Faculty, Supporting faculty, Outpatient timings, Services (Acute
dialysis, Maintenance dialysis, Paediatric Chronic Renal Failure Clinic (PCRF),
Renal transplant) Training programs, Collaborations, Memberships,
Conferences and events organised, Research projects – external and internal.
Areas of research, Future plans, Statistics, Some snapshots, Contact details.
(Website of 1St Primer on Pediatric
Renal Transplant IPNA -ISN -TTS Teaching Course:
http://www.pednephro.org).
Adolescent medicine
Adolescent medicine is a fairly young facility which was started in May 2013, as a sub-speciality of Paediatrics in the Department of Child Health. A team of paediatricians, paediatric nurses, psychologists and nutritionists cater to the healthcare needs of adolescents aged 10-19 years both in the outpatient setting and as inpatients.
Adolescents engage well with our team of healthcare providers as we ensure that an ‘alone interview’ happens during every visit, to facilitate rapport building and a safe space for teens to discuss sensitive health-related problems without fear of judgement. Indian law considers adolescents as ‘children’ till 18 years and there is no leeway for us to carry out this ‘alone interview’ without the permission of the parent. Our experience so far has been positive in that, no family member has prevented this interview from being conducted. Therefore, we have been able to give adolescent-friendly care on par with what is practised in the rest of the world.
Some of the problems that we manage include anorexia nervosa and other eating disorders, overweight and obesity, sleep problems, menstrual problems, poor scholastic performance, anxiety, depression, experimentation with substances, sexuality, teens with LGBTQ-related problems, contraception advice, teen pregnancy and family conflict. All teens irrespective of their clinical diagnosis, will have a HEADS screen done, and receive advice on healthy lifestyle, sexual health, safety, breast / testicular self-examination and vaccines. Towards caring for these teens, we collaborate closely with other departments within the institution, in particular Child and Adolescent Psychiatry and OG, governmental agencies and NGOs.
Patient story
Mumtaz (name changed) was managed recently in a multidisciplinary team effort, within and outside of the hospital. The story is in the words of the Director of a children’s home where she had stayed while receiving treatment in CMC.
“It was 9:30 PM on Sunday, 26 July, 2020. The CHILDLINE (this children’s home has been recognised as a subcenter for CHILDLINE) help desk team in Jolarpet railway station received a call from the Government Railway Police to attend to a 15-year-old girl who was wandering in the railway station late in the night. They were not sure how Mumtaz had reached the station since there was no transportation of any kind including trains during the peak of the pandemic-related lockdown.
Upon rescue, she was found to be cheerful but severely malnourished, in dirty clothes, her head covered by a cloth and flies swarming around her. Our team determined her to be from a state other than Tamil Nadu. As per protocol COVID test was done and found to be negative. She was found to have a huge gaping scalp wound, with pus and maggots in it. She was taken to the government hospital which is two hours away and admitted for further management.
At the hospital, her wound was cleaned and she was treated with strong antibiotics. After three days she was discharged with advice to continue daily dressings at home and a referral to the Plastic surgery department in the government hospital in Chennai. Considering the huge size of the wound, we sought help from the team of doctors in AMC, Department of Pediatrics, Christian Medical College, Vellore(CMC). She was admitted immediately under AMC, transfused two pints of blood and started on antibiotics and daily dressings. She was in their care for 10 days and began to interact and eat better. She was followed up in the AMC outpatient clinic, with discussions with plastic surgery and dietary departments.
Mumtaz was unable to give adequate contact details about her family, except that it was in another state. She seemed to be older than 15 years and bone age was done in CMC and age was determined to be approximately 22 years. Although our home is for children, we readily agreed to take care of her at the request of the Child Welfare Committee (CWC) and District Child Protection Unit (DCPU) of Vellore District.
At discharge, she was placed in our home, caregivers were trained by CMC staff on daily dressings and good nutrition was provided as recommended by the doctors. She was given a lot of TLC(tender loving care) in our home. She engaged well with the girls and began helping out in small activities. The staff did 24-hour shifts to be with her round the clock. CMC treated her during hospitalisation and the subsequent outpatient clinic visits free of cost. The trustees of the children’s home unanimously agreed to her care even though it was beyond the mandate.
When our search for her family started, we had interactions with police in a local police station closest to her village in the home state. We used video clips of Mumtaz to help the local police search for her family in her village. The police then spoke with her through a WhatsApp video call. To our pleasant surprise, a social worker living in a neighbouring village took interest in her case, called us and said that he had seen the video which the police had circulated. He had worked the whole of the previous night through WhatsApp groups. By morning Mumtaz’s family sent a small video for her to see. It was heartwarming for our staff to then watch Mumtaz speak with her family members. Within a week her father arrived in Vellore to take her home. After 52 days of stay with us and in the hospital, Mumtaz’s care was handed over to her dad in the presence of CWC and DCPU.
The
Department of Paediatrics provides holistic care for children with Cystic
Fibrosis (CF), a genetic disease that affects multiple organs and can be fatal
if left untreated. In this video , Mr. Hari Prathap Reddy, paediatric
respiratory therapist explains and demonstrates how chest physiotherapy should
be administered to children.
View the full playlist of chest physiotherapy videos
Playlist for nutritional management
of Cystic Fibrosis
Email us :
child1@cmcvellore.ac.in
04162283350
Mon-Fri: 8 am to 4.30 pm
( Sat : 8 am to 12:30 pm)