History of the Training Programmes under the Department of Critical Care:
Diploma in Critical Care 1997
In 1997, the Diploma in Critical Care for training of technicians was started with a view to train allied health personnel who were focused on the care of a critically ill patient.
Post Doctoral Fellowship program in Critical Care 2006
After the Department came together, a 2-year Post Doctoral Fellowship program in Critical Care was started in 2006 for trainees following completion of MD Medicine, Anaesthesia, Emergency Department and Respiratory Medicine. Currently, we have 5 Post doctoral fellowship seats.
Fellowship of the College of Intensive Care Medicine (FCICM) 2010
The department received accreditation from the College of Intensive Care Medicine (CICM, Australia and New Zealand) as a certified centre for training, in 2010 towards the Fellowship of the College of Intensive Care Medicine (FCICM) with Dr George John and Dr Peter John Victor, both FCICM graduates, as the initial Director and Supervisor of Training towards this course. Following this recognition, Dr Binila Chacko and Dr Pritish Korula (former SICU faculty) have completed their FCICM training. Currently, Dr Peter John Victor is the course director and Dr Binila Chacko is the Supervisor of Training towards this course.
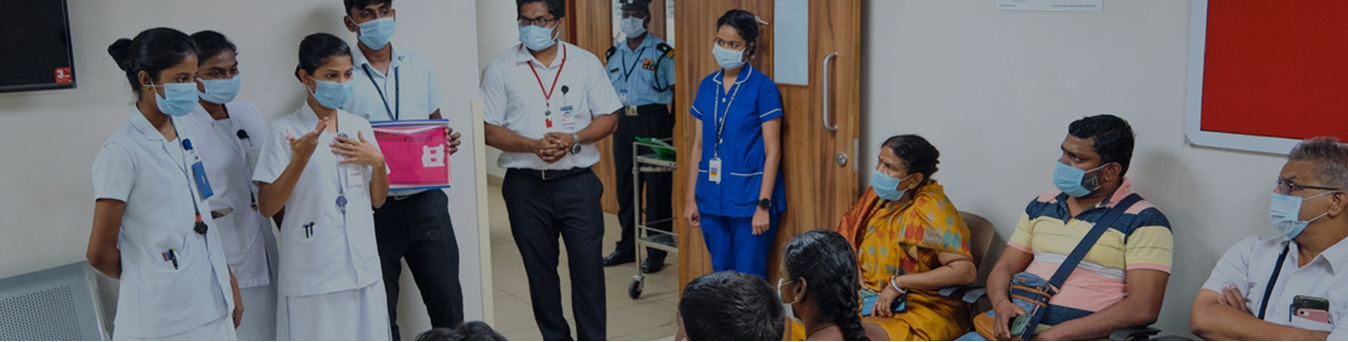
BSc Critical Care Technology 2012
In 2012, it was felt that the scope of the B. Sc respiratory therapy course, which was already in existence, was broader than critical care. This course included pulmonary function tests, sleep lab, and allergy testing, which were not necessary for a technical person who was to work exclusively in the intensive care unit. The Department of Critical Care at CMC Vellore hence submitted a request to the Tamil Nadu Dr. MGR Medical University to create a new course, BSc Critical Care Technology, to provide training to allied health personnel who were responsible for the care of critically ill patients. Currently, Mr Sam Prabhakaran from Medical ICU and Mr Baskaran from Surgical ICU are the course co-ordinators and Dr Thomas Isaiah and Dr Dhanoop Varghese are the faculty in charge of this course.
DM Critical Care 2015
The Medical Council of India (MCI) approved one DM seat for Critical Care Medicine on 21.9.2015. The PG Expert Group and the Board of Governors have recommended the recognition of this DM Critical Care seat on 11.2.2019, following the MCI inspection during the examination of the first candidate in August-2018. At this stage, Christian Medical College Vellore was the only college under the Tamil Nadu MGR university with this MCI recognised degree. From December 2020, the number of seats in the DM Critical Care program was increased from one to five. The initial cohort of five students successfully completed their course in January 2024.
IDCCM and IFCCM
In addition, the Indian Society of Critical Care Medicine (ISSCM) has acknowledged the Department for its 1-year Diploma course (IDCCM) and 2-year fellowship (IFCCM) programme. Furthermore, candidates have the option to enrol in the European Diploma in Intensive Care (EDIC) program after spending a year at the Department.
Current trainees:
At present there are 15 candidates enrolled for DM Critical Care Medicine, 5 for PDF (Post-doctoral fellowship in critical care), 5 for IDCCM and 30 ICU technician trainees for BSc in Critical Care Technology.
Email us :
micu@cmcvellore.ac.in
04162282693
Mon-Fri: 8 am to 4.30 pm
( Sat : 8 am to 12:30 pm)