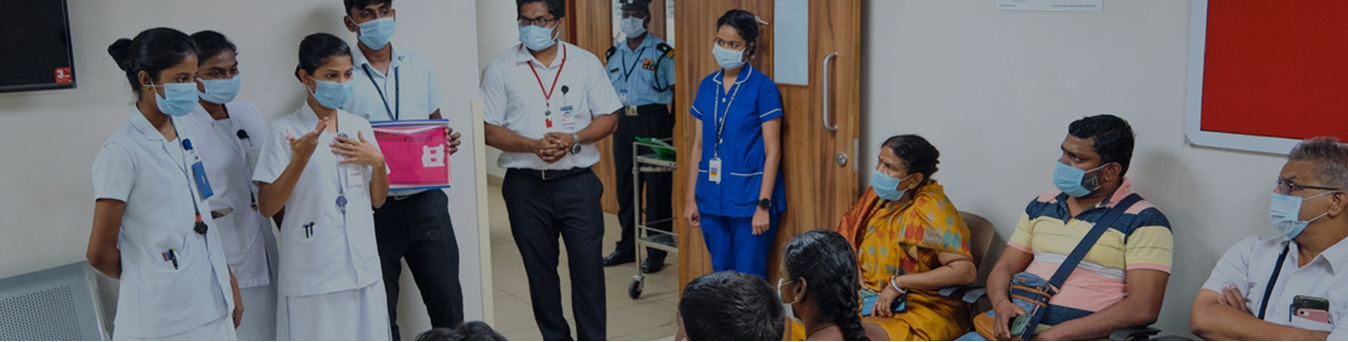
OPD Services
We offer outpatient services from Monday to Friday 8:00 am to 4: 30 pm. Appointments are with prior booking. Our OPD is located at G1, ground floor, OPD block (RT block).
OPD Schedule
In-patient services
Radiotherapy services
External Beam Radiation Therapy
Conventional Radiotherapy
3-Dimensional conformal radiotherapy (3D-CRT)
Intensity Modulated Radiation Therapy
Volumetric Modulated Arc Therapy (VMAT)
Image Guided Radiotherapy (IGRT)
Stereotactic Radiosurgery (SRS)
Stereotactic Radiotherapy (SRT)
Stereotactic Ablative Body Radiotherapy (SABR)
Total Body Irradiation (TBI)
Total Skin Electron Therapy (TSET)
Brachytherapy
Day Care Chemo
Quality Assurance and Dosimetry
Machine-specific QA
Patient-specific QA
In vivo Dosimetry
International Patients
For first appointment
Frequently asked questions
OPD Schedule
Day / Time
8: 00 am to 12:30 pm
12: 30 to 4:30 pm
Monday
RT Unit 2
(Head and neck, oesophagus, stomach, Lung cancers and cancers of prostate, urinary bladder and male genital tract)
RT Unit I
(Gynaecological, colorectal, Liver, pancreas and skin cancers)
Tuesday
RT Unit 3
(cancers of breast, brain, haematological malignancies, sarcomas and bone tumours, cancer in children)
RT Unit 3
(cancers of breast, brain, haematological malignancies, sarcomas and bone tumours, cancer in children)
Wednesday
RT Unit I
(Gynaecological, colorectal, Liver, pancreas and skin cancers)
RT Unit 3
(cancers of breast, brain, haematological malignancies, sarcomas and bone tumours, cancer in children)
Thursday
RT Unit 2
(Head and neck, oesophagus, stomach, Lung cancers and cancers of prostate, urinary bladder and male genital tract)
RT Unit 2
(Head and neck, oesophagus, stomach, Lung cancers and cancers of prostate, urinary bladder and male genital tract)
Friday
RT Unit I
(Gynecological, colorectal, Liver, pancreas and skin cancers)
RT Unit 3
(cancers of breast, brain, haematological malignancies, sarcomas and bone tumours, cancer in children)
In-patient services
We offer in-patient services for those patients who require Chemotherapy, supportive care during Radiation Therapy and Brachytherapy. Patients need to be seen by one of our doctors in the OP room or emergency room to get admitted in to our in-patient services.
Radiotherapy services
The department has the latest external beam Radiation Therapy treatment facility and Remote After-loading Brachytherapy facility. Patients from different parts of the country as well as international patients are referred to us so that they can have cost-effective “State of the Art” Radiation Therapy treatment. We have a Somatom Definition 4D-CT simulator (Siemens, Germany) for Radiation Therapy treatment planning. Image registration with CT, MRI as well as PET-CT can be done.
We have the CLINAC 2100 CD and TrueBeam STx linear accelerators (Varian Medical System, USA) in addition to the Theratron-80 Equinox telecobalt machine (Best Theratronics, Canada) and Microselectron (Nucletron, Holland) remote after-loading High Dose Rate (HDR) brachytherapy units. We use the Eclipse v13.7 treatment planning system (TPS, Varian Medical System, USA), Oncentra (Nucletron, Holland) TPS and Iplan TPS for treatment planning.
Our centre is a leading cancer institute in the country with facilities ranging from conventional radiation techniques to the latest high precision Radiation Therapy techniques such as 3D conformal, VMAT, IMRT, IGRT, SRS, SRT, SBRT, Total Body Irradiation and Total Skin Electron Therapy. The wide variety of available radiation delivery techniques offer personalized treatment to cancer patients depending on their tumor type, site, stage and general health. The radiation therapy is delivered either as in-patient or out-patient based on requirement.
About 7200 new patients were seen as out-patients and nearly 3400 patients were treated as in-patients in 2016-2017. More than 3200 patients were treated with radiation in the same year in our department.
External Beam Radiation Therapy
Conventional Radiotherapy:
Conventional radiotherapy or 2 –Dimensional radiotherapy is a time-tested and reliable radiation technique which offers cost-effective radiotherapy treatment using telecobalt unit or linear accelerator.
3-Dimensional conformal radiotherapy (3D-CRT):
As the name suggests, 3D-CRT helps to conform the shape of the radiation beam to the tumour tissue using multi-leaf collimators (MLCs). The treatment planning is done on CT data set which ensures that the tumour receives adequate dose while normal organs are spared, resulting in reduced treatment related side effects. About 400 patients are treated annually with 3D-CRT.
Intensity Modulated Radiation Therapy (IMRT):
IMRT is an advanced radiotherapy technique that uses sophisticated computer programs for inverse planning and dose calculation while delivering highly conformal radiation by modulating the intensity of radiation beam using multi-leaf collimator. IMRT helps increase the dose to tumor and further minimizes normal tissue doses, thereby, improving tumor control and reducing the side effects to the patient. IMRT is used to treat cancers of prostate, head and neck, lung, gastrointestinal and breast; and brain tumors as these tumors tend to be located close to critical organs. It may also be used to treat lymphoma, sarcoma, gynecologic cancers, and select pediatric cancers.
Volumetric Modulated Arc Therapy (VMAT):
VMAT is an advanced form of IMRT that delivers a precisely-sculpted 3D dose distribution with a full or partial rotation of the gantry in a single or multi-arc treatment. During conventional IMRT treatments, the linear accelerator makes repeated stops and starts to treat the tumor from a number of different angles while rotating around the patient. However, VMAT enables faster treatment with continuous dose delivery during rotational arcs in typically two minutes or even less.
Image Guided Radiotherapy (IGRT):
IGRT is the use of advanced imaging modalities with in-room imaging facilities to adjust for tumour motion or patient setup accuracy between treatments to augment target and normal tissue delineation, and potentially, to adapt treatment to tumor response. We use 2D-based kV and MV imaging or 3D-based Cone Beam CT which is most relevant in the treatment of tumour sites such as prostate, head and neck cancers and abdominal tumours.
Each year about 600 patients are treated with IMRT, VMAT and IGRT.
Stereotactic Radiosurgery (SRS):
Stereotactic radiosurgery is a highly precise technique that allows the delivery of high dose ionizing radiation to conform to a localized intracranial target volume, usually 1-3 cm in diameter. It uses multiple non-coplanar beams that point at the target centre which is positioned at the linac isocentre.
Linear accelerator-based SRS is used to treat both benign and malignant brain tumours. This procedure is done in collaboration with neurosurgery and more than 90 patients are treated every year using this technique.
Stereotactic Radiotherapy (SRT):
This offers multiple-fraction stereotactic treatment for suitable tumours. It is used to treat benign as well as malignant tumors located near critical sites in the brain. At least 100 patients are treated each year with SRT.
Stereotactic Ablative Body Radiotherapy (SABR):
SABR delivers high dose of radiation to tumor in 2-5 fractions while minimizing damage to healthy tissue. It involves the use of special immobilization and sophisticated image guidance that localizes the three-dimensional location of the tumor so that the radiation can be more precisely delivered. SABR is typically used to treat small early-stage lung cancer, prostate cancer, inoperable pancreatic cancer, liver cancer and cancers that have limited spread to the lung, liver or spine.
Total Body Irradiation (TBI):
TBI is primarily used as part of the preparative regimen for haematopoietic stem cell or bone marrow transplantation. It aims to deliver homogenous radiation dose to the entire body but limiting dose to the lungs. We are one of the leading centers in India practicing this complex treatment technique and treat about 70 patients per year.
Total Skin Electron Therapy (TSET):
TSET is a rare procedure for irradiating the skin of entire body using electrons. It is used for the treatment of mycosis fungoides and cutaneous T-cell lymphoma.
Brachytherapy:
Brachytherapy uses sealed radioactive sources placed within or near the tumor in the body using needles, catheters or surface moulds. This procedure delivers a high dose of radiation to the target with only a very minimal dose affecting the surrounding tissues.
This procedure requires specialized applications for each site under sedation or anesthesia and may require hospitalization. We have a Nucletron/Elekta remote after-loading High Dose Rate (HDR) Brachytherapy unit with Iridium-192 as the source and low-dose rate BARC applicators with Cesium-137 sources.
The common brachytherapy Techniques used are Intracavitary brachytherapy – (ICBT) for cancers arising from cervix including image guided brachytherapy (IGBT), vaginal mould brachytherapy, Interstitial brachytherapy using MUPIT and Vienna applicators for cancers such as cervix, vagina, anal canal etc. In addition, techniques such as intraluminal radiation therapy (ILRT) for cancer of the oesophagus, bronchus and biliary tree, Surface Mould brachytherapy for skin cancers and interstitial implant for breast and soft-tissue sarcoma are available.
Day Care Chemo:
We offer day care chemotherapy for patients who require concurrent chemotherapy. We have a well-equipped day care chemotherapy room with laminar air-flow facility manned by well-trained oncology nurses.
Quality Assurance and Dosimetry
In our institution we are concerned about the quality and consistency of treatment planning and delivery in all aspects of the radiotherapy process. We therefore routinely perform quality assurance procedures that reduces the uncertainties and errors in treatment planning and dosimetry to ensure consistency and accuracy over the planned course of medical prescription for all the patients. A team of medical physicists, who are responsible for commissioning of radiation equipment, calibration of dosimeters, maintaining personal monitoring devices and computing treatment plans involve in these activities, thereby, improving dosimetric and geometric accuracy and the precision of dose delivery.
Machine-specific QA:
Machine specific QA is performed on a routine basis to ensure that the accuracy, performance and constancy of the dose delivery of all therapy machines are within the tolerance limits. The machine-specific QA has an impact on the results of patient-specific QA and thus errors in patient-specific QA can be reduced to a minimum. Machine-specific QA are performed daily, weekly, monthly and annually.
Patient-specific QA:
Patient-specific QA is done to ensure that the delivered dose distribution agrees with the calculated dose distribution. Patient-specific QA is not only a clinical necessity but also a regulatory requirement. Currently, the 4D Octavius (PTW, Germany) which is a rotating phantom that accommodates an ionization-based detector array is used for 3D dose verification while radiochromic films (EBT 3) and portal dosimetry using EPID are used for 2D planar dose verification.
In vivo Dosimetry:
In vivo dosimetry is performed to measure and verify the dose delivered to the patient during the treatment. In vivo dosimeters such as Metal Oxide Semi-conductor Field Effect Transistor (MOSFET), Optically Stimulated Luminescent Dosimeter (OSLD), Thermo-luminescent Dosimeters (TLD) and diodes are either positioned on the patient’s skin or inside. In vivo dosimeters act as a useful tool in estimating the absorbed dose delivered, evaluating the dose to organs-at-risk and identifying deviations in the delivery of standard or complex treatments.
International Patients
Christian Medical College Hospital caters to patients from a total of 73 countries. The department provides out-patient and in-patient care to patients from various nations. An International Patient Office (IPO – 900) has been functioning in the premises of the erstwhile Ida Scudder Citizens’ Clinic building close to the CMC hospital exit gate for the benefit of our international patients. For outpatient appointments, online booking is available in the CMCH main web page or at the registration counters in the hospital premises. We strongly encourage you to travel using a valid Medical Visa and not to contact or make payment to touts for early appointments or other service promises.
For first appointment
For Web appointments – https://clin.cmcvellore.ac.in/webapt/
http://www.cmch-vellore.edu -> Are you a patient -> Book Appointments -> Appointment -> New International patient
For Queries – webappointment@cmcvellore.ac.in
At Counters – SILVER GATE (600) for private appointments and ISSCC building ground floor counters 2-10 for general appointments
Frequently asked questions
regarding International Patients
regarding Online Booking